 Understanding the Emerging Health Care Landscape
Understanding the Emerging Health Care Landscape
As the year 2026 unfolds, the landscape of health care in the United States is undergoing significant transformations. The ongoing dynamics of health, fitness, and overall wellbeing are profoundly influenced by recent legislative actions, both at the federal and state levels. Policymakers are acknowledging the imperative need to enhance coverage and access to health care services, all while managing the costs associated with these services. This critical juncture is pivotal for numerous stakeholders, including patients, health care providers, and insurance companies.
Recent federal initiatives aim to address key issues related to affordability, thereby encouraging more individuals to seek preventive care and maintain their fitness levels. Heightened emphasis on mental health, reproductive health rights, and chronic disease management are crucial areas where policy changes can make a significant impact. Such changes may lead to increased accessibility of services that facilitate a more comprehensive approach to health and fitness.
State governments are also actively participating in these shifts by implementing programs that expand Medicaid coverage and promote innovative public health strategies. As states adopt various models to improve healthcare delivery, the repercussions of these adjustments reflect the diverse needs across different populations. In a world where politics increasingly intertwine with health care policies, understanding the roles of local and federal governance is essential for navigating the changing environment.
In summary, the health care changes anticipated in 2026 present both challenges and opportunities. The focus on creating equitable access to quality health care can lead to improved health outcomes for many Americans. As stakeholders adapt to these evolving policies, it is crucial to remain informed and engaged in discussions surrounding the future of health care and the overall wellbeing of the population.
Impact of Expiration of ACA Subsidies
The expiration of enhanced subsidies under the Affordable Care Act (ACA) in 2026 is expected to have significant ramifications on the health care landscape in the United States. These subsidies have been pivotal in making insurance coverage more affordable for millions of Americans, thus promoting better health and wellbeing outcomes.
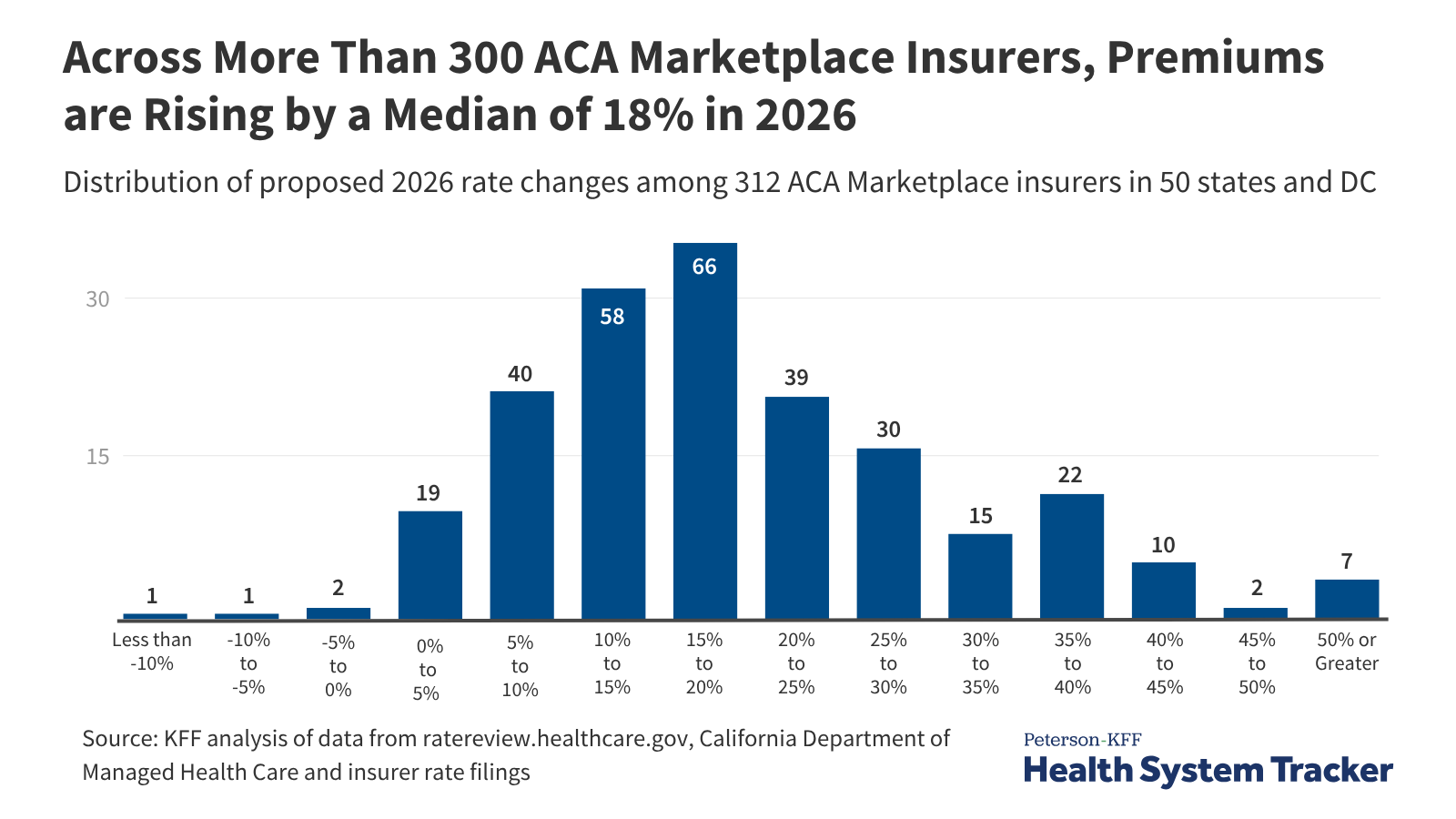
With the expiration of these financial aids, individuals who rely on ACA marketplace plans may face increased premiums that could rise dramatically. The loss of these subsidies means that many families, particularly those with low to moderate incomes, may find it unaffordable to obtain necessary health and fitness care. As a result, there is a growing concern that millions could potentially lose their health coverage, leading to an increase in the uninsured rate across the country. The inability to afford health insurance is likely to exacerbate existing health disparities and hinder access to preventive services.
Moreover, the absence of tax credits that previously helped offset insurance premiums may dissuade individuals from enrolling in plans altogether. High premiums can deter not only low-income populations but also those who are in need of regular health check-ups and fitness care. This may have a cascading effect on public health, as more individuals may forgo treatment for chronic conditions, leading to deteriorating health outcomes and increased strain on emergency services.
An analysis of potential changes in coverage highlights the need for policy discussions about future health reforms. It is essential to consider the implications of these policy changes on not only individuals but also on the broader healthcare system. There is an urgent need to either reinstate these subsidies or introduce alternative mechanisms to ensure that access to affordable health insurance is maintained in light of the expiration of these crucial provisions.
Key Provisions of the One Big Beautiful Bill Act of 2025
The One Big Beautiful Bill Act of 2025 introduces several transformative provisions aimed at enhancing health care coverage and access across the United States. A significant aspect of this legislation is the expanded eligibility for Health Savings Accounts (HSAs). This initiative allows a broader demographic to take advantage of tax-advantaged savings for medical expenses, ultimately fostering greater financial independence in health management. More individuals will be empowered to prioritize their health needs through these flexible savings options, improving overall wellbeing.
Moreover, one of the central changes pertains to the finance structure of Medicaid. The Act aims to increase federal support for state Medicaid programs, which has historically faced funding challenges. With increased financing, states are more likely to expand coverage under Medicaid, potentially leading to a larger population receiving essential health services. This financial bolstering offers states the opportunity to implement innovative care delivery methods, enhancing access, and promoting higher standards of care and fitness for Medicaid recipients.
In addition to financial adjustments, the Act addresses eligibility and work requirements in Medicaid programs. By reassessing these criteria, the One Big Beautiful Bill seeks to strike a balance between ensuring access to health coverage for those in need and maintaining accountability for individuals benefiting from public assistance. This approach may result in a more equitable system where health access is less contingent on bureaucratic processes, thus promoting better health outcomes and overall wellbeing among vulnerable populations.
Overall, the provisions introduced by the One Big Beautiful Bill Act of 2025 have the potential to reshape the landscape of health care in the United States, particularly in terms of coverage and accessibility for all citizens.
Revising Childhood Vaccine Recommendations
The landscape of childhood vaccinations is undergoing significant revisions, with a growing emphasis on a ‘shared clinical decision-making’ model. This shift is primarily aimed at enhancing individual parental involvement in health decisions while maintaining robust public health measures. For years, vaccines have played a crucial role in preventing infectious diseases among children, enhancing the overall health and wellbeing of the population. However, public health experts and pediatricians are now expressing concerns about potential implications related to this new framework.
At the core of this revised recommendation is the acknowledgment that parents should be actively involved in the health decisions concerning their children, especially concerning vaccinations. This approach intends to respect parental autonomy while ensuring they are informed about the benefits and risks associated with the vaccines. Advocates for this model argue that it can lead to better health outcomes and increased compliance, particularly among hesitant parents.
Nevertheless, the move towards shared decision-making has raised alarms in certain circles. Experts caution that diminishing the authority of health institutions may inadvertently reduce vaccination rates, possibly leading to the resurgence of preventable diseases. The effectiveness of vaccines is well-documented, yet public sentiment around health and fitness often reflects broader societal beliefs and misconceptions. Pediatricians worry that the new guidelines could foster an environment where vaccine hesitancy flourishes, ultimately jeopardizing the health of the community.
As discussions around these changes unfold, it is critical to strike a balance between respecting parental choices and preserving the integrity of public health initiatives. Maintaining high vaccination coverage is indispensable for preventing outbreaks of diseases like measles, whooping cough, and influenza, all of which pose considerable threats to children’s health. There is an urgent need for continued dialogue and education to ensure that the public understands the importance of vaccinations in promoting health and safeguarding wellbeing.
State-Level Legislative Changes
As of January 1, 2026, significant developments in state-level health care policies, particularly in Illinois, demonstrate a proactive approach to improving coverage and access to care. These changes aim to enhance the health and wellbeing of residents while tackling various facets of health care delivery, including insurance and drug costs. With these legislative updates, Illinois joins the broader movement of states supporting local health initiatives that align with federal reforms.
One notable law focuses on increasing transparency within the insurance marketplace. By mandating that insurers clearly disclose premium costs, deductibles, and out-of-pocket expenses, residents can make informed decisions regarding their health care coverage. This transparency is crucial for both consumers and health care providers, as it fosters trust and accountability in the health system.
Additionally, Illinois has enacted legislation aimed at reducing drug costs for patients. This initiative involves creating a database to monitor price fluctuations and ensuring that patients have access to essential medications without excessive financial burden. This approach not only promotes health equity but also enhances the overall efficacy of the state’s healthcare system by reducing barriers to necessary treatment.
Moreover, changes in care delivery methods have also been introduced. Illinois has prioritized telehealth services, allowing for increased access to care, especially in underserved areas. Telehealth has proven vital during the COVID-19 pandemic and continues to be an essential aspect of a multifaceted health care strategy. By expanding telehealth options, the state addresses the needs of individuals who may encounter obstacles in accessing traditional healthcare services.
These legislative changes in Illinois exemplify how state governments are taking a leading role in shaping the future of health and fitness policy. By aligning closely with federal efforts while tailoring solutions to local needs, states can significantly contribute to the overall improvement of health and wellbeing within their communities.
Emerging Trends in Digital Health
The healthcare landscape is evolving, particularly in response to emerging health policies aimed at enhancing accessibility and affordability. As the demand for efficient care increases, digital health platforms are becoming essential tools in the healthcare environment. These platforms facilitate a variety of urgent care and behavioral health services, ultimately diminishing the financial burden on patients.
One significant trend is the rise of telemedicine, which allows patients to consult with healthcare providers remotely. Telehealth services are essential during times of crisis, such as the recent global pandemic, where in-person visits could pose risks. By offering virtual consultations, digital health innovations not only provide crucial services but also help maintain continuity of care, which is vital for overall wellbeing.
Furthermore, the integration of artificial intelligence (AI) in health management systems offers predictive analytics that enhance patient care. AI can facilitate personalized experiences by analyzing patient data to recommend tailored treatment plans. This personalized approach can lead to improved health outcomes and reduced costs, showcasing how technology plays a pivotal role in reshaping healthcare delivery.
Another emerging trend is the use of mobile health applications that promote health and fitness by empowering individuals to track their health metrics. These applications often include features such as medication reminders and wellness coaching, enabling users to take charge of their health journey. By incorporating fitness tracking and well-being monitoring into everyday life, these tools not only support individual health management but also contribute to public health efforts.
The adoption of digital health platforms reflects a broader commitment to making healthcare more accessible and affordable. With ongoing advancements and policy support, the future of healthcare appears poised to leverage technology in ways that enhance patient experiences and improve outcomes.
Impact of Federal and State Reforms on Access and Affordability
The landscape of health care in the United States is in a constant state of evolution, influenced significantly by both federal and state reforms. As we look towards 2026, it is crucial to understand how these changes might reshape access to affordable care and overall provider operations. Federal reforms, particularly those aimed at universal coverage, are likely to enhance the accessibility of health services for diverse population groups. Policies that encourage the expansion of Medicaid and subsidized insurance options typically aim to reduce the burden of health care costs for low- and middle-income families, thereby improving their health and fitness outcomes.
On the state level, there is substantial variability in how reforms are implemented, which can significantly impact local health care markets. Some states may opt to introduce innovative health care delivery models that focus on integrated care, thus improving patient access and promoting better wellbeing. Additionally, state-level policies that regulate insurance premiums and provider reimbursements can directly affect affordability—for instance, limiting out-of-pocket expenses for essential health services like preventive care, mental health support, and chronic disease management.
Furthermore, market innovations such as telemedicine, digital health platforms, and personalized health management tools are emerging as vital components of a reformed health care system. These innovations can enhance patient engagement, streamline access to services, and lower costs by reducing unnecessary in-person visits. However, the effectiveness of these reforms will largely depend on the collaboration between federal and state governments to create a cohesive policy framework that addresses both access and affordability comprehensively.
Ultimately, as we approach 2026, understanding the intertwined effects of federal and state reforms on health care access and affordability will be essential for stakeholders. By examining these elements, we can better prepare for the potential long-term implications of changes in health policy on our communities.
Stakeholder Reactions and Legislative Tracking
The shifting landscape of health care policy in 2026 has elicited a variety of responses from key stakeholders, including patients, health care providers, and policymakers. These groups are deeply invested in understanding the implications of recent legislative changes on coverage, access, and overall health outcomes.
Patients, who are the most affected by these policies, have expressed mixed feelings. Many are concerned about the potential reduction in coverage options and the impact on their overall wellbeing. Patient advocacy organizations have mobilized to ensure that the voices of those affected are heard, emphasizing the need for equitable access to health services. Alongside patients, health care providers are closely monitoring the changes. They are particularly focused on how the new regulatory framework will influence their practice environments, reimbursement models, and patient care strategies.
Policymakers are also actively tracking these developments, recognizing that midterm elections can significantly affect health policy direction. Legislative monitoring is paramount, as bills related to insurance markets and Medicaid are likely to shape the future of health care accessibility. Stakeholder engagement in this process is critical, as these groups aim to influence legislation by advocating for policies that promote health and fitness across diverse populations.
Furthermore, the integration of technology in health care delivery continues to garner attention from stakeholders. Innovations aimed at enhancing healthcare access, such as telemedicine platforms, are being closely examined for their potential to improve patient experiences amidst the evolving policies. Stakeholders are also leveraging data to track outcomes related to legislative changes, with a unified goal of ensuring that every individual can achieve optimal health and wellbeing.
Conclusion: The Future of Health Care Policy
As we navigate the evolving landscape of health care policy in 2026, it becomes imperative to acknowledge the significant shifts that have already begun to reshape coverage and access for individuals across the United States. The interplay of health, fitness, wellbeing, and politics within this sphere underscores the complexity surrounding the provision of health care services. Critical reforms, alongside emerging technologies and innovative practices, are anticipated to serve as catalysts for improving health outcomes.
The focus on preventive care, mental health support, and the integration of holistic well-being within traditional health care frameworks reflects an essential shift towards a more comprehensive understanding of what constitutes health. Policies that emphasize these aspects not only highlight the importance of physical health but also recognize the interconnectedness of emotional and social well-being, which are crucial for an improved quality of life.
Moreover, the continuous monitoring of policy implications is vital as we observe the impact of these reforms on diverse populations. Stakeholders, including lawmakers, health care providers, and communities, must engage in collaborative efforts to ensure that advancements in health care are equitable and accessible to all. This necessitates an ongoing dialogue about potential barriers and solutions that may emerge in the coming years.
Looking ahead, it is essential for those involved in health care policy to remain agile and responsive to change. By staying informed about advancements in health, fitness, and wellbeing, and considering how these dynamics intersect with political actions, we can better forecast the trajectory of health care policy. In conclusion, the future of health care provision is contingent upon our ability to adapt and innovate, ensuring that all individuals receive the care they need to thrive.

















 Los Angeles | Redlands | Phoenix | Memphis | NYC
Follow us: @GemworkTV | Contact: info@gemwork.tv
Los Angeles | Redlands | Phoenix | Memphis | NYC
Follow us: @GemworkTV | Contact: info@gemwork.tv